ACUPUNCTURE FAQ
A MINIMALLY INVASIVE AND EXTREMELY SAFE PROCEDURE THAT AWAKENS, STRENGTHENS, AND FOCUSES THE BODY’S CAPACITY TO HEAL ITSELF
Over two thousand years ago, Hippocrates (considered by many to be the father of Western medicine) stated: “Natural forces within us are the true healers of disease.” Now in the twenty-first century, scientists all over the world are scrambling to explain how acupuncture works, with varying degrees of success. Though they are discovering bits and pieces of the answer, the bottom line is this: the way that acupuncture works is to enhance, strengthen, and direct these “natural forces”.
Contrary to what you may have heard, acupuncture is NOT a belief system, a religion, superstition, or magic. You don’t need to “believe” in it in order for it to work. Though it seems foreign and mysterious to many Westerners, modern acupuncture is a minimally invasive and extremely safe procedure that stimulates the nervous system and connective tissue in ways that no other intervention can—no medication, therapy, or surgery can do what acupuncture does.
I could talk all day long about what is amazing and wonderful about acupuncture! Below I have compiled detailed answers to the most common questions that I’ve encountered in my nearly 20 years of practice. You can find information about cost and insurance here. If you have a question that isn’t addressed, please reach out so that we can help you.
Does acupuncture hurt?
The simple answer to this question is “no”. Most first time patients are surprised and pleased to find that acupuncture treatment is a relaxing and pleasant experience.
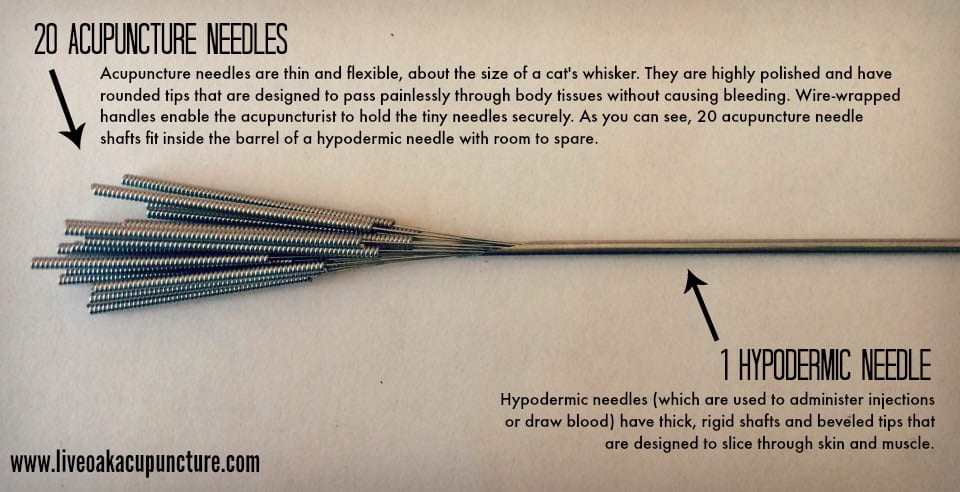
It is important to understand that acupuncture needles are nothing like the needles used to administer injections or collect blood (called hypodermic needles). Hypodermic needles have thick, rigid shafts with an angled tip that is designed to slice through skin and muscle (see size comparison to the right). In contrast, acupuncture needles are very thin – about the diameter of a cat’s whisker. Because they are so thin, acupuncture needles are very flexible. In addition, they have a highly polished surface and a rounded tip that is designed to pass painlessly through the skin and body tissues without causing damage or bleeding.
Many patients do not experience any sensation when the needle penetrates the skin, but some people feel a prick similar to a mosquito bite or a mild stinging sensation. When the needle reaches the correct depth, some patients feel a dull ache, a tingling sensation, or a sense of distention under the skin. This sensation dissipates quickly, and most patients experience a sense of deep relaxation and calmness for the remainder of the treatment. Many patients actually fall asleep while the acupuncture needles are in place.
How many treatments will I need?
This is one of the first questions that most people considering acupuncture have. We are all busy and money doesn’t grow on trees. It is natural to feel impatient and to hope for a dramatic and rapid results from a new treatment.
The short answer to this question is that an “average” initial course of treatment consists of eight to ten sessions, with most people noticing a clear benefit within three to four sessions. Usually during the initial course of treatment sessions are scheduled on a weekly basis, although in severe cases more frequent treatments are necessary.
Many chronic problems (for example back pain of several years’ duration, lifelong seasonal allergies, or persistent insomnia) require multiple courses of treatment before it is possible to transition to maintenance care. In contrast, acute problems (for example a recent ankle sprain or a bout with influenza) typically require fewer treatments, in many cases two or three are adequate.
It is important to remember — you didn’t get this way overnight and you are not going to heal overnight either. Acupuncture is like eating well or working out — you can’t do it just once and expect it to have a significant and lasting impact on your health. I am results-oriented and my goal is to get you to the point that you can stop treatment or transition to maintenance care as quickly as possible. On the other hand, without exception my patients who have had the best results and who have gone on to truly “graduate” from their pain and health problems are those who have patiently committed to consistent treatment.
THE SPECTRUM OF ACUPUNCTURE RESPONSE
It is difficult to predict up front how quickly your body will respond to acupuncture. About 10% of people are what we call “acupuncture strong responders”. This means that they will notice dramatic and lasting benefit from just a few sessions. On the other end of the spectrum is about 10% of people who we consider “acupuncture non-responders”. These people will not benefit from acupuncture, no matter how many treatments they receive. The remaining 80% of people fall somewhere between these two extremes.
If you are going to respond to the therapy, you can expect to see some positive changes within 3-4 sessions. This does not mean that your symptoms are gone within this period of time, only that your pain or symptoms are less severe, you are sleeping more restfully, your mood is brighter, you are having more “good days” than you did before, etc. This is an encouraging result which suggests that will continuing care you will experience more and more relief.
PHASES OF TREATMENT
Children or young people in good health with acute problems (for example a cold or minor ankle sprain) often only require 2-3 treatments. Older individuals and those with chronic health problems typically require a longer course of treatment. In these cases, treatment is divided into three phases:
- Acute care – During this phase, treatments are scheduled weekly (or 2-3 times per week in severe cases). The goal during this phase is to relieve symptoms and to start the process of addressing the underlying cause of pain or health problems.
- Convalescent care – During this phase, treatments are usually scheduled every two weeks. The goal during this phase is to maintain symptomatic relief while focusing on resolving underlying disharmonies and preventing future problems.
- Maintenance care – During this phase, treatments are scheduled once a month or four times per year (usually at the change of seasons). The goal during this phase of care is to maintain the progress we have made and to support your vitality and overall wellbeing.
FACTORS THAT GO INTO DETERMINING HOW MANY TREATMENTS YOU WILL REQUIRE
The length of time you spend in each phase depends on a number of factors, including:
1. Whether your problem is acute or chronic
2. How long you have had the problem
3. Whether you can avoid the conditions that caused your problem
4. Your age
5. Your general state of health
6. How readily your body responds to acupuncture (see above)
7. Whether or not you follow the instructions you are given regarding diet and lifestyle
Progress will be faster if you faithfully follow your treatment plan by keeping your appointments, taking your herbal medication every day (if applicable), and following any advice that you are given about dietary or lifestyle changes. Click here to learn about The Three Free Therapies — things that you can do at home to minimize the number of treatments you will require.
Once I start, do I have to get acupuncture forever?
One of the biggest myths about acupuncture is that “once you start, you have to go forever.” Perhaps the most apt analogy for continuing care for the meridian system is reconstructive orthodontics for your teeth. Both disciplines consist of an initial phase of care that usually involves overcoming a weakness, followed by a reconstructive or rehabilitative phase of care, and finally culminating in wellness or maintenance.
Frequent visits in the initial phases of treatment
The earliest phase of your care usually consists of the highest visit frequency. In cases of chronic imbalances within the meridian system it is common to initially require treatments a few days a week until your bodies energy is properly balanced and restored. Using our orthodontic analogy, this would be the point at which the brackets and wires are put on your teeth and you are seen for check-ups every couple weeks. Since there is no wire affixed within your meridian system, your acupuncture visits occur more frequently than orthodontic appointments, and are instead “wired together” by specific exercises, herbal prescriptions, self-care recommendations, etc.
Less frequent visits during maintenance care
As balance returns to your body, your visit frequency is diminished. This is the phase in which the orthodontist would also begin spacing out his visits and begin to “tweak” the wires to make fine adjustments to your teeth and allow them to settle into their new structural pattern. In both cases, this is a critical phase of care in that it is setting the stage for lifelong wellness or maintenance. In regard to orthodontics, this is when you would be fitted for a retainer to be worn at least nightly for the rest of your life, or for as long as you wish to maintain healthy, straight teeth. As for acupuncture, this marks the transition to a schedule of wellness or maintenance care to ensure a lifelong abundance of health and well-being. The maintenance or wellness phase of care is without a doubt the most important. What is sickness but a lack of wellness? The whole objective of everything leading up to your wellness care is to get your body back to its natural state of balance. Once there, staying well is simply a matter of sustaining that balance.
Is acupuncture relevant in the modern world?
One of the most exciting aspects of Chinese Medicine is that it is particularly well suited to treating stress-related ailments that are so common today. According to Dr. Donald E. Kendall:
“The Chinese recognized that so-called civilization was contrary to natural living, and brought with it certain strains and stresses, which they called ‘the dust’ – possibly a reference to the dusty conditions of overcrowded ancient cities. The treatment for stress was known as ‘wiping away the dust’. The risks to health are much the same today, and include the physical and emotional stress caused by living in large complex societies, overcrowding, adverse environmental factors, air pollution, poor water quality, bad eating habits, overeating, alcohol and drug use, smoking, lack of exercise, overwork, and poor sleeping habits. As a consequence, heart disease, cancer, diabetes, infertility, impotence, asthma, allergic disorders, gastrointestinal and urogenital disorders, acute and chronic pain, arthritis, rheumatism, anxiety, and depression, among others, are widespread. These diseases represent a general malaise of civilization, and no single medical approach can solve all these problems for all people. Chinese medicine has survived for many centuries for the very reason that it has been effective in addressing a wide range of human ailments, including those mentioned above.”
– Dr. Donald E. Kendall
Chinese medicine offers a coherent explanation for many common “modern” health concerns
Unlike conventional medicine, Chinese medicine offers a coherent theory regarding the cause and treatment of many of these stress-related health concerns (see for instance Emotions As the Primary Cause of Disease). While conventional medicine offers drugs to suppress symptoms, Chinese medicine offers an explanation of how modern living causes these problems and how they can be effectively treated with dietary changes, herbs, and acupuncture. The cause and treatment of many common health concerns can be clearly explained by Chinese medicine and can be effectively treated with safe and relatively low-cost modalities such as herbs and acupuncture. This offers hope to many Americans who have struggled for years with “incurable”, “idiopathic”, or “unexplained” conditions such as:
- Menstrual and hormonal problems, including painful periods and PMS.
- Menopausal complaints.
- Female and male infertility.
- Migraine headaches.
- Fibromyalgia and chronic fatigue syndrome.
- Autoimmune diseases.
- Allergies and asthma.
- Irritable bowel syndrome.
- Depression and anxiety.
- Insomnia.
- Chronic pain.
What conditions does acupuncture help with?
“What is it that we want? To fully experience our aliveness. To feel in our bodies a streaming, like a river over stones. To be awake, alert, and responsive in our limbs and sensitive in our fingertips. To feel as if our inner and outer reality is congruent and that our efforts are rewarded by a sense of satisfaction. We aspire to have our private lives nestle within the valley of a public world which we can affirm. We long to feel connected with each other. We want to be able to embrace and be embraced. We want to live the life of our bodies and want our bodies to permit us to fully live our lives. Chinese medicine is a beginning.”
– Harriet Beinfield and Efrem Korngold in Between Heaven and Earth: A Guide to Chinese Medicine
There are seven key benefits of acupuncture:
- Relieves pain
- Enhances immune function
- Regulates and balances hormones
- Elevates mood
- Relaxes muscles
- Eliminates stress
- Enhances mental clarity
Because it stimulates the body’s ability to heal itself, acupuncture is a valuable complement to conventional medical treatment of almost any condition.
Click here for an introduction to acupuncture from the National Center for Complementary and Alternative Medicine.
In 2002, the World Health Organization published a comprehensive review and analysis of controlled clinical trials on acupuncture. The authors of the review analyzed over 300 studies of acupuncture, and categorized the various conditions that were studied into four groups: (1) diseases, symptoms, or conditions for which acupuncture has been proved – through controlled clinical trials – to be an effective treatment; (2) diseases, symptoms, or conditions for which the therapeutic effect of acupuncture has been shown but for which further proof is needed; (3) diseases, symptoms, or conditions for which there are only individual controlled trials reporting some therapeutic effects, but for which acupuncture is worth trying because treatment by conventional and other therapies is difficult; and (4) diseases, symptoms, or conditions for which acupuncture may be tried, provided the practitioner has special modern medical knowledge and adequate monitoring equipment.
Diseases, symptoms, or conditions for which acupuncture has been proved – through controlled clinical trials – to be an effective treatment:
- Adverse reactions to radiation or chemotherapy
- Allergic rhinitis (including hay fever)
- Biliary colic (pain from gallstone attack)
- Depression
- Dysentery (disease which causes inflammation of the large intestine, leading to diarrhea, abdominal pain, vomiting, and fever)
- Dysmenorrhea (painful periods)
- Epigastric pain (including peptic ulcer, acute and chronic gastritis, and gastrospasm)
- Facial pain (including craniomandibular disorders)
- Headache
- Hypertension (elevated blood pressure)
- Hypotension (decreased blood pressure)
- Induction of labor
- Knee pain
- Leukopenia (reduced number of white blood cells)
- Low back pain
- Malposition of fetus (breech)
- Morning sickness (nausea in pregnancy)
- Nausea and vomiting
- Neck pain
- Dental pain (including temporomandibular joint dysfunction)
- Periarthritis of the shoulder
- Postoperative pain
- Renal colic (pain from kidney stones)
- Rheumatoid arthritis
- Sciatica
- Sprain
- Stroke
- Tennis elbow
Diseases, symptoms, or conditions for which the therapeutic effect of acupuncture has been shown but for which further proof is needed:
- Abdominal pain
- Acne
- Alcohol dependence and detoxification
- Bell’s palsy (one-sided facial paralysis resulting from damage to the 7th cranial nerve)
- Bronchial asthma
- Cancer pain
- Cardiac neurosis (chest pain caused by stress)
- Cholecystitis (gallbladder inflammation)
- Cholelithiasis (gall stones)
- Competition stress syndrome
- Craniocerebral injury, closed
- Diabetes mellitus, non-insulin dependent (adult-onset diabetes)
- Ear ache
- Epidemic hemorrhagic fever
- Epistaxis, simple (nose bleed)
- Eye pain
- Female infertility
- Facial spasm
- Female urethral syndrome
- Fibromyalgia
- Gastrokinetic disturbance
- Gouty arthritis
- Hepatitis B carrier status
- Herpes zoster (shingles)
- Hyperlipidemia (elevated cholesterol)
- Hypo-ovarianism (deficient hormonal activity of the ovaries)
- Insomnia
- Labor pain
- Lactation, deficient (inadequate breast milk production)
- Male sexual dysfunction, non-organic
- Meniere’s disease (vertigo)
- Neuralgia, post-herpatic (persistent pain following shingles)
- Neurodermatitis
- Obesity
- Opium, cocaine, and heroin dependence
- Osteoarthritis
- Pain due to endoscopic examination
- Pain in thromboangiitis obliterans
- Polycystic ovarian syndrome (a hormonal disorder that is associated with ovarian cysts, irregular ovulation, infertility, male-pattern hair growth, and obesity)
- Postextubation in children
- Premenstrual syndrome
- Prostatitis, chronic (inflammation of the prostate)
- Pruritis (itchy skin rash)
- Radicular and pseudoradicular pain syndrome (pain due to irritation of a spinal nerve)
- Raynaud’s syndrome (cold and discolored fingers or toes due to inadequate circulation)
- Recurrent lower urinary tract infection
- Reflex sympathetic dystrophy (dysfunction of the nervous system that causes severe pain and progressive disability)
- Retention of urine, traumatic
- Schizophrenia
- Sialism, drug-induced (excessive salivation)
- Sjogren syndrome (autoimmune disorder in which the glands that produce tears and saliva are destroyed)
- Sore throat
- Spine pain, acute
- Stiff neck
- Temporomandibular joint dysfunction
- Tietze syndrome (inflammation of the ligaments that connect the sterum and ribs)
- Tobacco dependence
- Tourette’s syndrome (disorder that involves tics and involuntary sounds and compulsive rituals or behaviors)
- Ulcerative colitis, chronic (inflammation and ulcers of the large intestine)
- Urolithiasis (kidney stones)
- Vascular dementia (dementia due to vascular disease)
- Whooping cough (pertussis)
Diseases, symptoms, or conditions for which there are only individual controlled trials reporting some therapeutic effects, but for which acupuncture is worth trying because treatment by conventional and other therapies is difficult:
- Cholasma (hyperpigmentation of the skin, sometimes associated with pregnancy)
- Choroidopathy, central serous (fluid accumulation under the retina caused by leakage from the blood vessel under the retina)
- Color blindness
- Deafness
- Hypophrenia (low IQ)
- Irritable bowel syndrome
- Neuropathic bladder in spinal cord injury (reduced bladder capacity or incomplete bladder emptying)
- Pulmonary heart disease, chronic
- Small airway obstruction
Diseases, symptoms, or conditions for which acupuncture may be tried, provided the practitioner has special modern medical knowledge and adequate monitoring equipment:
- Angina pectoris (chest pain due to cardiovascular disease)
- Breathlessness in chronic obstructive pulmonary disease
- Coma
- Convulsions in infants
- Diarrhea in infants and young children
- Encephalitis, viral
- Paralysis, progressive bulbar and pseudobulbar (neurological disorder which causes weakness and spasticity of the muscles of the pharynx, larynx, and tongue)
I have pain. How can acupuncture help me?
Acupuncture Helps With Three types of pain
Although acupuncture is effective for a wide variety of conditions, it is mostly widely renown in the United States as a treatment for pain. In general, there are three types of pain patients who walk in the door of an acupuncture clinic:
- Patients with acute pain – This type of pain is typically the result of an injury. A good example would be an ankle sprain. In this case, pain serves as an alarm that signals you to rest and protect the painful area long enough for it to heal. In a way that is not yet understood by science, acupuncture effectively speeds the healing process and often enables patients to comfortably return to their regular activities in less than half the time that would have been required to heal the injury without acupuncture. In an otherwise healthy patient, often only a handful of acupuncture sessions are required to treat an episode of acute pain.
- Patients with pain resulting from overuse – This type of pain is actually a sub-type of acute pain. In this case, there is not a single injury that caused the pain, rather the problem is the result of chronic overuse of a joint, muscle, or region of the body. This overuse is most commonly associated with a person’s occupation — carpal tunnel among administrative assistants, wrist pain among new mothers, shoulder pain among hairstylists, back pain among mechanics. In an ideal world, this type of pain would also serve as a signal from the body to rest and avoid the demands that caused the pain in the first place, but such rest is not possible for many people because avoiding the cause of the pain would mean quitting a job or neglecting other important responsibilities. In cases of overuse-related pain, acupuncture can be very helpful in reducing pain to a much more tolerable level, but in most cases ongoing treatment is required in order to maintain relief.
- Patients with chronic pain – Although many people (including a lot of physicians) don’t realize it, chronic pain is unfortunately an entirely different and much more complicated condition than acute pain. The most current neurological research indicates that when pain persists for an extended period of time it causes irreversible changes to the parts of the central nervous system (the brain and spinal cord) that transmit and perceive pain signals. Rarely are there simple answers to chronic pain (always be very suspicious of anyone who claims to offer one). The goal of treatment in cases of chronic pain is effective management and improvement of quality of life (as opposed to cure) and this generally requires a multi-pronged approach. Treatments that may be a part of this approach include acupuncture, prescription medication, exercise, meditation, massage, physical therapy, counseling, and/or other modalities.
HOW DOES ACUPUNCTURE IMPROVE QUALITY OF LIFE IN CHRONIC PAIN PATIENTS?
Acupuncture can absolutely make a life-changing difference in cases of chronic pain, but in many cases becoming completely and permanently pain-free is an unrealistic goal for the chronic pain patient. I am always up-front with new patients who come to me with chronic pain — acupuncture is not going to be an overnight fix. At least four treatments are generally required in order to assess whether a particular individual will respond to acupuncture and an initial course of 10-12 sessions will likely be required to bring about lasting relief. Some type of maintenance treatment is almost always required — the goal is to arrive at a maintenance schedule that requires visits only every month or two, but this is not always possible (particularly in patients with other major health problems or when chronic pain is very widespread).
BENEFITS OF ACUPUNCTURE FOR CHRONIC PAIN
With patience and persistence, acupuncture can offer chronic pain patients:
- Reduced pain
- Enhanced response to medication (enabling patients to get the same relief from less pain medication)
- Improved sleep
- Relief from depression and/or anxiety
- Elevation and stabilization of mood
- Enhanced energy
All of this adds up to an important improvement in quality of life. Even if a portion of their pain persists despite acupuncture treatment, most individuals with chronic pain find that their ability to live with their pain is dramatically improved when they are sleeping restfully; when their mood is lightened; when they have the energy and focus to return to work, hobbies, and family responsibilities; and when they are able to reduce their reliance on pain medications (and therefore reduce the severity of side effects that typically accompany those medications).
I’m having a hard time getting pregnant. Can acupuncture help me?
“I would like to personally endorse Kristen Horner as an extremely knowledgeable practitioner in the area of women’s health. Kristen performed an intensive one-on-one internship with me addressing women’s reproductive health. In addition to her knowledge of Traditional Chinese Medicine in treating women’s physical issues, she also embodies a depth of compassion in dealing with the mental and emotional difficulties women may experience in their own healing process. She is a true healer.”
– Randine Lewis, Ph.D., L.Ac., author of The Infertility Cure
Acupuncture and Chinese herbal medicine provide effective solutions for the following women’s health concerns
- Painful periods and endometriosis
- PMS
- Irregular cycles
- Menstrual migraines
- Menopausal symptoms
- Hormonal imbalance
Chinese medicine also offers proven benefits for couples seeking pregnancy, including:
- Improved ovarian function and production of better quality eggs.
- Increased blood flow to the uterus and increased thickness of the uterine lining.
- Regulation of hormones.
- Prevention of uterine contractions during early pregnancy.
- Decreased chance of miscarriage.
- Improvement of quantity and quality of sperm.
- Regulation of the immune response.
- Induction of ovulation and regulation of the menstrual cycle.
- Relaxation for the patient and reduction of stress.
- Elimination of underlying inflammation that may impair fertility.
- Increased quantity and quality of cervical mucus.
My colleague Dr. Attilio D’Alberto has compiled an excellent summary of the current research regarding acupuncture and Chinese herbal medicine for infertility.
Comments from Patients
“After five years of trying to get pregnant, my husband and I had nothing to lose, so I called Kristen to try acupuncture. Within 3 months of starting treatment I was pregnant! Not only was my body in better condition, but my mind and emotions were, too. I don’t know exactly how it works, but I was amazed that after five years of infertility, including much stress and many expenses at other doctors, within three months using acupuncture with Kristen, I was pregnant. Whatever she did worked and I am so grateful.”
-A.A. (baby girl born 11/2006)
“My experience working with Kristen Horner to treat my infertility was very positive as well as beneficial — I truly believe that her treatments helped me get pregnant. I was very impressed with her vast knowledge of both Eastern and Western medicine, as well as her willingness to integrate both viewpoints and to work with my OB/GYN and his treatment plan.”
-B.M. (baby girl born 5/2007)
“After many months of struggling with fertility drugs and depression, I decided to give acupuncture a try and called Kristen on my doctor’s recommendation. Within a few weeks of beginning treatment I felt healthier, slept better, and felt more like myself again. After only a month of working with Kristen, I became pregnant and am now anxiously awaiting the arrival of my first child! Kristen was a tremendous source of support and knowledge for me and I feel extremely fortunate to have met her. I highly recommend her and believe that God has given her an incredible capacity to help others.”
– N.P. (baby girl born 3/2007)
“I have suffered from severe endometriosis for many years, but I noticed improvements in my condition after my first session with Kristen. With ongoing acupuncture and herbal medicine, I have continued to improve and how have the most pain-free periods of my life. I am so happy I no longer have to plan my life around my period!”
– C.S.
“I did a lot of research beforehand and I am so happy that I decided to call Kristen! I have had problems with fibromyalgia which was also causing my anxiety and depression, IBS and PMS with severe cramping. I have tried medications (all had uncomfortable side effects to say the least), chiropractors and was even contemplating surgery. Within a month I had complete relief from my PMS and my IBS. I have been going to see Kristen now for 3 ½ months, and my fibromyalgia pain is no longer bothering me. My anxiety and depression are much better as well. I can finally sleep better at night and I have a lot more energy during my day, which is very important so I can keep up with my toddler. Something that I was not intending to fix with acupuncture, my bunion on my left foot has completely gone away as well! I am so glad I did not spend the money on a podiatrist before going to see Kristen. I also take herbal supplements that have made a tremendous difference overall. Even my 2 year old daughter takes the herbal allergy medicine which has no side effects like her regular prescription drug does.”
– D.E.
“What led me to try acupuncture was over a year of chronic knee pain, diagnosed as Iliotibial Band Syndrome. I had done months of physical therapy, gotten two MRI’s, seen two orthopedic surgeons—none of whom were able to figure out the source of my knee pain. Kristen listened to my concerns and helped me understand my body more holistically. She linked my knee pain to other problems I have struggled with, such as chronic constipation and an unexplained absent menstrual cycle. With several weeks of Chinese herbs and acupuncture my digestion is now functioning normally, my period has returned after an absence of 4 years, and my knee has greatly improved and is on it’s way to full recovery. I am very thankful for Kristen’s help and willingness to see me and my body as a whole.”
– E.V.
Will acupuncture help me lose weight?
ACUPUNCTURE IS NOT A MAGIC BULLET FOR WEIGHT LOSS
One of the most common questions that I hear is “does acupuncture help with weight loss?” The answer is yes, but in most cases not nearly as fast and not to the extent that most people are hoping. (I do not offer ear stapling or stimulant herbal formulas. While these methods may offer quick weight loss, they do so at the risk of serious side effects.)
It is very common for people to come to me for other concerns (such as back pain, allergies, or insomnia) and, after several months of treatment, report that they have lost 20 pounds without really trying. The reason that this happens is that acupuncture reinforces physiological balance and, as a result, strengthens your body’s ability to provide you clear feedback regarding its dietary needs.
HOW ACUPUNCTURE MIGHT HELP YOU LOSE WEIGHT
When they are getting acupuncture, people notice that:
- They feel satisfied with less food.
- Their junk food cravings go away.
- They start developing a preference for healthy food.
- They start feeling very unpleasant when they overeat or eat unhealthy food.
- They stop engaging in emotional eating.
- If pain was previously impairing their ability to exercise, pain relief as a result of acupuncture enables them to be more active.
Gradually, over the course of weeks and months, these changes add up to a real difference on the scale.
ACUPUNCTURE IS JUST ONE PIECE OF THE PUZZLE
The problem is that these changes are subtle, especially initially, and it takes time for a deficit of a few hundred calories a day to add up to a change in the way your clothes fit or the number on the scale. Ultimately, when people lose weight using acupuncture, the weight loss is very healthy because it takes place gradually and is the result of a real lifestyle change (as opposed to a short-term gimmick).
The downside is that, if you are looking to lose 30 pounds in 30 days, acupuncture is not the right treatment for you and you will almost certainly be disappointed.
If you are interested in losing weight, my recommendation is that you view acupuncture as one piece of the puzzle, not a magic bullet. Commit to a course of acupuncture therapy with the knowledge that it is a whole body treatment is similar to eating healthy and exercising in the sense that it needs to be carried out over time in order to see change.
Is acupuncture safe?
Like any medical procedure, acupuncture is not entirely without risk. Fortunately, injuries are extremely rare among patients treated by trained practitioners. In the United States, acupuncturists use factory-sterilized, single-use, disposable needles. The needles are individually packaged according to strict government guidelines and are discarded immediately after use, so there is no risk of disease transmission.
In a Japanese survey of 55,291 acupuncture treatments given over five years by 73 acupuncturists, 99.8% of them were performed with no significant minor adverse effects and zero major adverse incidents (Hitoshi Yamashita, Bac, Hiroshi Tsukayama, BA, Yasuo Tanno, MD, PhD. Kazushi Nishijo, PhD, JAMA). Two combined studies in the UK of 66,229 acupuncture treatments yielded only 134 minor adverse events. (British Medical Journal 2001 Sep 1). The total of 121,520 treatments with acupuncture therapy were given with no major adverse incidents (for comparison, a single such event would have indicated a 0.0008% incidence).
Common, minor adverse events
A survey by Ernst et al. of over 400 patients receiving over 3500 acupuncture treatments found that the most common adverse effects from acupuncture were:
- Minor bleeding after removal of the needles, seen in roughly 3% of patients. Holding a cotton ball for about one minute over the site of puncture is usually sufficient to stop the bleeding.
- Bruising, seen in about 2% of patients. Bruising usually go away after a few days. This side effect is more common among patients taking blood thinning medications such as Coumadin, warfarin, Plavix, or anti-inflammatory drugs.
- Dizziness, seen in about 1% of patients. Some patients have a conscious or unconscious fear of needles, which can produce dizziness and other symptoms of anxiety. Patients are usually treated lying down in order to reduce likelihood of fainting. Being careful to eat a light meal or snack prior to treatment significantly reduces the likelihood of this type of problem
The survey concluded: “Acupuncture has adverse effects, like any therapeutic approach. If it is used according to established safety rules and carefully at appropriate anatomic regions, it is a safe treatment method.”
Risks from omitting orthodox medical care
Receiving any form of alternative medical care without also receiving orthodox Western medical care can be inherently risky, since undiagnosed disease may go untreated and could worsen. For this reason I prefer to consider acupuncture a complementary therapy rather than an alternative therapy, and always encourage my patients to remain under the care of their physicians.
Safety compared with other treatments
Commenting on the relative safety of acupuncture compared with other treatments, the NIH consensus panel stated that “adverse side effects of acupuncture are extremely low and often lower than conventional treatments.” They also stated: “the incidence of adverse effects is substantially lower than that of many drugs or other accepted medical procedures used for the same condition. For example, musculoskeletal conditions, such as fibromyalgia, myofascial pain, and tennis elbow… are conditions for which acupuncture may be beneficial. These painful conditions are often treated with, among other things, anti-inflammatory medications (aspirin, ibuprofen, etc.) or with steroid injections. Both medical interventions have a potential for deleterious side effects but are still widely used and are considered acceptable treatments.”
My physical therapist or doctor says that I should get dry needling? What is that?
WHAT IS DRY NEEDLING?
Dry needling is a type of acupuncture that is rapidly gaining popularity. It involves the precise insertion of acupuncture needles into tiny tight wads of muscle called trigger points. Trigger points are found within taut bands of muscle and are often located in areas far from the location of the pain that causes a patient to seek treatment.
When a needle is inserted at just the right spot the result is a noticeable twitch of the muscle. By mechanisms that are not completely understood, this so-called local twitch response calms the confused electrical signals within the muscle that were holding the muscle fibers in contracture and reduces the concentration of a number of irritating chemicals that are present within trigger points. This leads to immediate reduction of local and referred pain, improved range of motion, decreased irritability of trigger points both in the area that was needled and elsewhere, normalized the pH within the muscle, and restored blood circulation.
IS DRY NEEDLING ACUPUNCTURE?
According to modern medical experts as well as historians, it is not unreasonable to speculate that acupuncture may have been developed thousands of years ago as a treatment for what we now know as trigger points. Although the term “trigger point” was coined by Dr. Janet Travell in the 1940s, the Chinese medical literature described the phenomena of tight bands muscle bands, tender knots within muscles that refer pain to distant locations, and needling as a treatment for the problem as early as the first century BCE. For this reason and others many experts and organizations, including the World Health Organization, classify dry needling as a sub-type of acupuncture.
For thousands of years, Chinese medicine has treated trigger points with acupuncture. Travell began needling trigger points with syringes in 1942, injecting them with procaine. Procaine was later replaced by saline solution,which was later replaced by “dry needling”—without any fluid in the syringe—bringing the procedure full circle to what is essentially acupuncture. – John M. McPartland, DO, MS
WHAT CAUSES TRIGGER POINTS?
Trigger points result when a muscle is overloaded, either suddenly or chronically. All people have at least a few trigger points, given that so many common situations cause them. Potential causes of trigger points include:
- Maintaining an awkward position too long
- Poor lifting habits
- Carrying an overloaded purse
- Bad posture
- Sitting on a wallet in the back pocket
- Hitching up your hip to carry a child
- Sitting at a computer for too long
- Any type of repetitive motion
- Poorly designed shoes
- Limping
- Falls
- Car accidents
- Abnormal bone structure (short arms, one leg that is longer than the other, an asymmetrical pelvis, etc.)
ARE TRIGGER POINTS A COMMON CAUSE OF PAIN?
In their seminal two-volume textbook on trigger points, Travell and her co-author Dr. David Simons state that trigger points are a component of 93% of the pain seen in pain clinics and are the sole cause 74% of the time. According to dry needling expert Jan Dommerholt,
“Myofascial trigger points are one of the most overlooked and ignored causes of acute and chronic pain, and at the same time constitute one of the most common musculoskeletal pain conditions.”
Perhaps part of the reason that trigger points are a under-recognized and under-treated cause of pain is that no medical specialty “claims” muscles as their domain. Virtually every other organ system has a medical specialty to diagnose and treat its dysfunction — neurologists and neurosurgeons treat the brain and nervous system, orthopedists treat bones, nephrologists treat kidneys, gastroenterologists treat the digestive organs, etc. but no medical specialty claims muscle as its primary domain. Although the increased popularity of dry needling has generated controversy over which professionals should be allowed to do it, hopefully one very positive thing that will come of it is increased attention to trigger points as a cause of stubborn, mysterious, and previously “untreatable” pain.
FINDING A WELL-TRAINED PRACTITIONER OF DRY NEEDLING
At this point in time there is controversy over which professionals should be allowed to practice dry needling. Dry needling is clearly within the scope of practice of licensed acupuncturists and, although not all acupuncturists use this technique, many are masterful practitioners of it (although they may call it by other names, including sports acupuncture, ashi acupuncture, or trigger point acupuncture).
There are numerous dry needling training programs available to physical therapists of widely varying quality and rigor. In 2012 I personally attended a very poor dry needling course for physical therapists and wrote about the experience in this article. I have since attended a course offered by another company and, although the second course was much better than the first, I still have serious concerns about physical therapists using this modality with only a few days training. The American Association of Medical Acupuncturists (AAMA) shares my concern and stated in a recent position paper that only licensed acupuncturists or medical doctors should perform dry needling:The AAMA strongly believes that, for the health and safety of the public, this procedure should be performed only by practitioners with extensive training and familiarity with routine use of needles in their practice and who are duly licensed to perform these procedures, such as licensed medical physicians or licensed acupuncturists. In our experience and medical opinion, it is inadvisable legally to expand the scope of physical therapists to include dry needling as part of their practice.
Many states (including Texas) do not offer clear guidance about how many hours of training in needling physical therapists must have in order to use the technique, with many states leaving it up to the individual physical therapist (or his or her employer) to determine whether they are “competent” with the technique. In the absence of a standardized dry needling credential or clearly defined training requirements for physical therapists, individual patients are left to ask careful questions of their physical therapist if dry needling is suggested. Questions patients should consider asking include:
- How many hours of training in the use of needles have you had?
- How many of these hours were hands-on versus classroom hours?
- How many patients have you treated under the direct supervision of a dry needling expert?
- How many patients have you personally treated with needles?
- Does your malpractice insurance policy explicitly cover dry needling?
In an effort to provide my patients with the very best care, in addition to 3000+ hours of acupuncture training, I have sought advanced training in dry needling.
Can kids get acupuncture?
CAN KIDS GET ACUPUNCTURE?
Yes, acupuncture is an ideal treatment for many childhood ailments.
Really?! Kids can get acupuncture?
Yes! Acupuncture works by activating and focusing the body’s own self-healing capacity and, because children’s self-healing capacity is much stronger than that of most adults, we often see remarkably quick and dramatic treatment results in children. While many adults have physical or emotional health problems are very firmly entrenched, children often require much shorter courses of treatment. Acupuncture can heal the root cause of your child’s health problem and save your child years or even decades of suffering.
How old does a child have to be to get acupuncture?
All ages of children, even newborns, can get acupuncture.
But doesn’t it hurt? I don’t want my child to be traumatized.

We use the very teeny, tiniest needles for children. Many kids do not feel anything at all when the needles are inserted. If there is any discomfort it only lasts for a brief moment. Voa, pictured at right, has been getting acupuncture since she was two years old. Her two favorite activities each week are going to the library for story time and coming to my office for her acupuncture appointment. To me this is great evidence that acupuncture is not painful or scary for children — most kids LOVE acupuncture.
IS ACUPUNCTURE SAFE FOR KIDS?
According to a study published in 2011 called “The Safety of Pediatric Acupuncture: a Systematic Review” in the journal Pediatrics, acupuncture was found to be safe when performed by an appropriately trained and licensed acupuncturist. In this study the authors focused on the safety of acupuncture in children by reviewing over 37 different studies on pediatric acupuncture. What they found was that acupuncture was extremely safe with little or no adverse reactions, especially when compared to many common over-the-counter drugs (such as acetaminophen). Researchers discovered that out of the combined studies’ nearly 1500 children and teenagers only a small percent (0.1%) experienced mild side-effects (such as bruising or a little bit of swelling at the needle site). Only in rare cases did serious adverse events occur and serious adverse events only occurred when the child was treated by an assistant or practitioner who wasn’t fully trained and licensed in acupuncture. As long as you are taking your child to a fully trained and licensed acupuncturist your child will be completely safe.
What pediatric conditions are treatable with acupuncture?
According to Pediatric Acupuncture: a Review of Clinical Research, there is scientific evidence for the effectiveness of acupuncture in treating the following conditions in children:
- Chronic Pain
- Pediatric Migraine
- Procedural Stress
- Enuresis (bedwetting)
- Constipation
- Epilepsy
- Allergies
- Neurologic Disability
- Laryngospasm
- Post-Operative Vomiting
- Cancer-related conditions
Where do you put the needles?
The placement of needles is determined on a case-to-case basis, but in almost every case I place a majority of needles in areas that are far from the site of pain or dysfunction. For example, when treating headaches I needle the feet, when treating back pain I treat the hands, and when treating digestive problems I needle the forearms.
I use a unique style of acupuncture referred to as Tung’s Magic Points, which is based on the teachings of Master Ching-Chang Tung (1916 – 1975). Dr. Tung was the recipient of a secret acupuncture point system, refined and handed down in his family over the course of nearly two thousand years. Master Tung has been referred to as the greatest acupuncture technician who ever lived. During his lifetime Dr. Tung treated hundreds of thousands of patients and gained fame for the amazing results he would obtain using just a few needles. After fleeing to Taiwan during the Cultural Revolution in China, Master Tung began to teach his secret acupuncture point system to select students, revealing his secrets outside his family for the first time. Even now only a tiny portion of this priceless knowledge is available in print and continues to be transmitted primarily as an oral tradition from teacher to student.
In 2007 I had the good fortune to complete a year of advanced training with Susan Johnson, who is the primary student of Dr. Miriam Lee (1949 – 2009), the first practitioner to bring Tung’s Points to the United States in the early 1980s and a key figure in the legalization of acupuncture in this country.
Tung’s Points are unique in that a smaller number of needles are used and all needles are placed in areas other than the site of pain or dysfunction. For example back pain is treated with needles in the hands and feet. Advantages of this approach include faster, more thorough resolution of pain and other health problems, and the fact that the patient can be comfortably positioned in a recliner chair and can generally be treated without removing clothing. Patients find this type of treatment much less anxiety-provoking than conventional acupuncture because they are not subject to needling in areas that already feel vulnerable because of injury, disease, or pain.
What type of education does a licensed acupuncturist have?
In order to be eligible for licensure, an acupuncturist must complete an accredited graduate-level degree program in Acupuncture or Traditional Chinese Medicine, pass three rigorous national certification examinations administered by the National Certification Commission on Acupuncture and Oriental Medicine (NCCAOM), pass written and practical portions of the Clean Needle Technique examination administered by the Council on Colleges of Acupuncture and Oriental Medicine, submit proof of malpractice insurance, and be approved for licensure by the Texas State Board of Medical Examiners.
Graduate-level degree programs in Acupuncture or Traditional Chinese Medicine entail 2800-3400 hours of specialized instruction and extensive supervised clinical practice (3-4 years of full-time study). A practitioner who has passed the NCCAOM acupuncture examination is entitled to add Dipl. Ac. (Diplomate of Acupuncture) after their name and a practitioner who has passed the NCCAOM herbal examination is entitled to add Dipl. CH (Diplomate of Chinese Herbology) after their name. The highest level of board certification is the Dipl. OM (Diplomate of Oriental Medicine) — practitioners with this designation have passed written and practical examinations on acupuncture, Chinese herbal medicine, and Western biomedicine.
Although some other healthcare professionals (such as medical doctors, doctors of osteopathy, and chiropractors) have the legal ability to practice acupuncture, it is important to recognize the vast discrepancy between the acupuncture training required of Licensed Acupuncturists versus other health professionals. In most states, medical doctors and doctors of osteopathy are allowed to practice acupuncture without any training whatsoever in Traditional Chinese Medicine, while chiropractors are required to complete only 100 hours of training (usually completed over the course of several weekends). Unfortunately, the limited training of other healthcare professionals in acupuncture often leads to a “cookbook” approach to treatment. Although this approach may bring about some benefits, acupuncture and Chinese herbal medicine only reaches its fullest degree of effectiveness when it is practiced by an individual with extensive training in the detailed and subtle system of TCM diagnosis and treatment.
DO YOU HAVE TO GO TO SCHOOL TO BECOME AN ACUPUNCTURIST?
Three or four years of graduate-level education are required to become a Licensed Acupuncturist
In order to be eligible for licensure, an acupuncturist must complete an accredited graduate-level degree program in Acupuncture or Traditional Chinese Medicine, pass three rigorous national certification examinations administered by the National Certification Commission on Acupuncture and Oriental Medicine (NCCAOM), pass written and practical portions of the Clean Needle Technique examination administered by the Council on Colleges of Acupuncture and Oriental Medicine, submit proof of malpractice insurance, and be approved for licensure by the Texas State Board of Medical Examiners. Graduate-level degree programs in Acupuncture or Traditional Chinese Medicine entail 2800-3400 hours of specialized instruction and extensive supervised clinical practice (3-4 years of full-time study). A practitioner who has passed the NCCAOM acupuncture examination is entitled to add Dipl. Ac. (Diplomate of Acupuncture) after their name and a practitioner who has passed the NCCAOM herbal examination is entitled to add Dipl. CH (Diplomate of Chinese Herbology) after their name. The highest level of board certification is the Dipl. OM (Diplomate of Oriental Medicine) — practitioners with this designation have passed written and practical examinations on acupuncture, Chinese herbal medicine, and Western biomedicine.
Other healthcare providers using acupuncture have much less training in the use of needles
Although some other healthcare professionals (such as medical doctors, doctors of osteopathy, and chiropractors) have the legal ability to practice acupuncture, it is important to recognize the vast discrepancy between the acupuncture training required of Licensed Acupuncturists versus other health professionals. In most states, medical doctors and doctors of osteopathy are allowed to practice acupuncture without any training whatsoever in Traditional Chinese Medicine, while chiropractors are required to complete only 100 hours of training (usually completed over the course of several weekends). Unfortunately, the limited training of other healthcare professionals in acupuncture often leads to a “cookbook” approach to treatment. Although this approach may bring about some benefits, acupuncture and Chinese herbal medicine only reaches its fullest degree of effectiveness when it is practiced by an individual with extensive training in the detailed and subtle system of TCM diagnosis and treatment.
I am a Christian. Is acupuncture against my religion?
The short answer to this question is “no”.
For a much more in-depth answer, please read this recent three-part blog series.
Is acupuncture just a placebo?
A recent study comparing real acupuncture, laser acupuncture, and sham laser acupuncture with no treatment for knee arthritis showed that real acupuncture, laser acupuncture, and sham laser acupuncture all resulted in decrease in pain. In the media this study has been presented as evidence that acupuncture does not work and that any decrease in pain associated with acupuncture is the result of the placebo effect. In reality the story is more complicated than that. First of all, the study was small, with fewer than 20 patients in each treatment group. Second, treatment was only administered for three months, which is rarely long enough to bring about lasting improvement in a condition that has, in most cases, developed over the course of decades. And third, the discussion of this study in the mainstream media and scientific circles ignores the fact that EVERY medical or surgical treatment relies quite heavily on the placebo response, whether we are talking about prescription medication, herbal medicine, acupuncture, or surgery.
Do I have to stop seeing my doctor or taking my medications to get acupuncture?
Absolutely not.
Western medicine does many things extremely well
Modern Western medicine has changed the world by achieving many amazing triumphs over disease, and Western medicine is the best choice when it comes to the treatment of acute infections, traumatic injury, situations which require surgery, and other illnesses such as cancer. Fortunately, Western medicine has tools at its disposal to actually cure these conditions by killing bacteria, repairing traumatic injury, repairing congenital or acquired malformation of organs or tissues, and stopping the spread of malignant tumors.
Chinese medicine fills in the gaps Western medicine leaves
On the other hand, most physicians will admit that there are a number of health problems that are not addressed particularly well by modern Western medicine. In the case of many chronic diseases and disorders, Western medicine offers only palliative care – meaning that symptoms are temporarily relieved with medication or surgery but the underlying cause remains.Examples of such chronic conditions include:
- Allergies
- Asthma
- Insomnia
- Depression
- Anxiety
- Chronic fatigue
- PMS
- Menstrual pain and irregularity
- Back pain
- Attention deficit disorder (ADD)
- Many others
In these cases, Chinese medicine offers a mode of treatment that effectively addresses the root cause of the disorder, while at the same time alleviating symptoms. In many cases, Chinese medicine can be used very effectively as an adjunct or complement to conventional Western care. My background in both Chinese medicine and Western science uniquely qualifies me to offer patients the best of both worlds.
How does acupuncture work?
Over two thousand years ago, Hippocrates (considered by many to be the father of medicine) stated: “Natural forces within us are the true healers of disease.” Now in the twenty-first century, scientists all over the world are scrambling to explain how acupuncture works, with varying degrees of success. Though they are discovering bits and pieces of the answer, the bottom line is this: the way that acupuncture works is to enhance, strengthen, and direct these “natural forces”.
Contrary to what you may have heard, acupuncture is NOT a belief system, a religion, superstition, or magic. You don’t need to “believe” in it in order for it to work. Although acupuncture may seem mysterious, the mechanism behind its effectiveness is quite simple. A basic understanding of two concepts is essential to understanding acupuncture. These concepts are Qi and Meridians.
Although it is unfamiliar to most westerners, Qi not a spiritual or a “new age” concept. One translation of the word Qi is “that which animates life”—the presence of Qi is what distinguishes a living person or animal from a dead person or animal (or an inanimate object). Qi is the motive force behind your ability to move, see, hear, heal, digest, and speak. It is the “spark” that keeps your heart beating, your blood circulating, and your brain thinking. It is the energy behind the phenomenal growth of a small child and the remarkable ability of the human body to heal from injury and disease. The main point when trying to grasp the concept of Qi is to consider the possibility that there is an immaterial level of reality that Western science cannot yet quantify or categorize. Acupuncture theory suggests that many of our physical and emotional problems begin at the level of function that is more subtle than our brain chemistry and organ function.
“From the standpoint of Western medical science, Qi is likely to be revealed as some amalgam of endorphins, the bioelectric potential of cell membranes, nervous conduction, circulating hormones and perhaps even photons (light) and infrared radiation (heat). In attempting to define and quantify qi, acupuncture research may end up identifying a whole new system of biological information, such as the conduction of impulses through the body’s connective tissue.”
– Arthur Rosenfeld
“Qi is understood to be the intrinsic, dynamic, self-regulating and self-maintaining power of the organism. All healing in Chinese Medicine is directed, ultimately, at conserving, protecting, augmenting, restoring, and facilitating Qi.”
– Harriet Beinfield & Efrem Korngold
Quantum physics has come to a similar understanding of the material world and the human body by proving that when we break down any material object into its smallest components, it is reduced to pure energy. Our bodies, while seemingly solid, are actually energetic configurations that are constantly changing. Acupuncture is premised on this understanding. The point of treatment is to manipulate the flow of Qi within our bodies in different ways to induce a therapeutic effect. By working on the energetic level, the physical and material levels can be directly affected. In fact, according to acupuncture theory, many forms of imbalance or disease cannot be fully healed simply by intervening on the material level. The underlying energetic component has to be addressed in order to treat the root cause of the problem.
Meridians (also known as channels) are the pathways that conduct Qi throughout the body. Free flow along the fourteen major and innumerable minor meridians of the human body brings life-giving Qi to every cell of your body, including the muscles, nerves, and organs. An obstruction in a meridian is like a dam in a river – Qi builds up and overflows the normal boundaries of the meridian on one side; on the other side tissues lack nourishment. When there is an obstruction, energy stagnates on either side of the blockage and tissue function is impaired. If the blockage is sustained, pain and disease is the result. In Chinese there is a saying, “If there is pain, there is no free flow; if there is free flow, there is no pain.”
Blockages can be caused by injury, contagious diseases, emotional stress, lack of physical activity, excessive physical activity, overuse injuries, faulty diet, and many other factors. Acupuncture and Chinese herbal medicine are used to remove blockages, regulate Qi, and restore physiological and psychological equilibrium.
To learn more about Qi and the other vital substances, click here.
Is there any scientific evidence that acupuncture works?
Below, the Acupuncture Now Foundation (ANF) has put together examples of specific studies on acupuncture together with links to those studies.
COST EFFECTIVENESS:
We chose to start this sampling of studies with ones of acupuncture’s cost effectiveness because it answers two important questions at once; if acupuncture can demonstrate cost effectiveness and the larger question of if acupuncture itself is clinically effective. Any therapy demonstrating cost effectiveness could only do so if that therapy was clinically effective.
A systematic review of cost-effectiveness analyses alongside randomised controlled trials of acupuncture.
Kim SY1, Lee H, Chae Y, Park HJ, Lee H.
Acupuncture Med. 2012 Dec;30(4):273-85. doi: 10.1136/acupmed-2012-010178. Epub 2012 Oct 25.
Abstract: http://www.ncbi.nlm.nih.gov/pubmed/23099289?dopt=Abstract
Full study: http://aim.bmj.com/content/30/4/273.long
Summation: 17 studies were included from Europe and Asia that looked at cost-effectiveness analysis, cost-utility analysis, and cost-benefit analysis for allergic rhinitis, dysmenorrhea, osteoarthritis, and headache. All cost utility analysis studies showed that acupuncture with or without usual care was cost-effective compared with waiting list control or usual care alone. Nine were CUAs that measured quality-adjusted life years (QALYs) and eight were CEAs that assessed effectiveness of acupuncture based on improvements in clinical symptoms. The cost-effectiveness analysis studies acupuncture was beneficial at a relatively low cost.
Costs and consequences of acupuncture as a treatment for chronic pain: a systematic review of economic evaluations conducted alongside randomised controlled trials.
Ambrósio EM1, Bloor K, MacPherson H.
Complement Ther Med. 2012 Oct;20(5):364-74. doi: 10.1016/j.ctim.2012.05.002. Epub 2012 Jun 6..
Abstract: http://www.ncbi.nlm.nih.gov/pubmed/22863652?dopt=Abstract
Full article: http://www.complementarytherapiesinmedicine.com/article/S0965-2299(12)00080-5/fulltext
Summation: A UK study using 8 economic evaluation studies, seven cost-utility analyses and one cost-effectiveness analysis covering the conditions of low back pain, neck pain, dysmenorrhoea, migraine and headache, and osteoarthritis. In the UK their National Institute for Health and Clinical Excellence sets a threshold for the cost of a quality adjusted life year (QALY) of £20,000 to £30,000. If a therapy can provide 1 QALY for less than £20,000 to £30,000, it is considered cost effective. In the seven cost-utility analyses, acupuncture was found to be clinically effective but cost more. The cost per quality adjusted life year (QALY) gained ranged from £2527 to £14,976 per QALY well below the threshold. The one cost-effectiveness study indicated that there might be both clinical benefits and cost savings associated with acupuncture for the treatment of migraine headache.
Acupuncture in patients with dysmenorrhea: a randomized study on clinical effectiveness and cost-effectiveness in usual care
Claudia M. Witt, MD, MBA, Thomas Reinhold, MSc, Benno Brinkhaus, MD, Stephanie Roll, MSc, Susanne Jena, MSc, Stefan N. Willich, MD, MPH, MBA
American Journal of Obstetrics and Gynecology
February 2008Volume 198, Issue 2, Pages 166.e1–166.e8
Abstract: http://www.ajog.org/article/S0002-9378(07)00920-9/abstract
Full article: http://www.ajog.org/article/S0002-9378(07)00920-9/fulltext
Summation: 649 women with dysmenorrhea were randomized to acupuncture (15 sessions over three months) or to a control group (no acupuncture) with 201 randomized. The average pain intensity on a 1-10 scale was lower in the acupuncture group (average 3.1) compared to the non-acupuncture group (average 5.4). The acupuncture group had better quality of life with the overall cost of ICER €3,011 per QALY).
MODES OF ACTION/MECHANISMS OF ACUPUNCTURE
The two most researched areas of the physiological actions and pathways underpinning acupuncture to date have been the analgesic/antihyperalgesic and anti-inflammatory effects of acupuncture.
The following are three excellent reviews of much of the evidence regarding how acupuncture relieves pain and/or inflammation via a multitude of mechanisms of internal signals causing adjustments of bodily resources.
Mechanisms of Acupuncture-Electroacupuncture on Persistent Pain (Review)
Ruixin Zhang, Ph.D., Lixing Lao, Ph.D. Ke Ren, Ph.D., and Brian M. Berman, M.D. Anesthesiology. 2014 Feb; 120(2): 482–503 .
Full article: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3947586/
Summation: This excellent review not only summarizes how studies in the last decade have found that acupuncture and electro-acupuncture cause the production of natural (endogenous) pain modifying substances including opioids, serotonin, and norepinephrine, it also details how recent research is finding the most effective frequencies (Hz ranges) for stimulating the production of these substances. Especially important in this time of an opioid epidemic in North America, recent research found that electro-acupuncture combined with very low dosages of analgesics provided greater relief than the acupuncture or medications alone.
Acupuncture: Emerging evidence for its use as an analgesic (Review)
GAO P, GAO X, FU T, XU D, WEN Q. Experimental and Therapeutic Medicine. 2015;9(5):1577-1581. doi:10.3892/etm.2015.2348.
Full article: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4471669/
Summation: Many studies have looked at how acupuncture causes pain relief (analgesia) and it has been hypothesized that acupuncture acts on various parts of the central nervous system, including the spinal cord, brain stem, cerebral ganglia and cerebral cortex. The complex mechanisms behind just how acupuncture causes these effects include neurohormones and neurotransmitters, such as endogenous opioids and γ-aminobutyric acid, as well as signaling pathways and even the immune response.
Mediators, receptors and signalling pathways in the anti-inflammatory and antihyperalgesic effects of acupuncture (Review)
John L. McDonald, Allan W. Cripps, and Peter K. Smith
Evidence-Based Complementary and Alternative Medicine, vol. 2015, Article ID 975632, 10 pages, 2015. doi:10.1155/2015/975632.
Full article: http://www.hindawi.com/journals/ecam/2015/975632/
Summation: Acupuncture has been used for millennia to treat allergic diseases including both intermittent rhinitis and persistent rhinitis. Besides the research on the efficacy and safety of acupuncture treatment for allergic rhinitis, research has also investigated how acupuncture might modulate immune function to exert anti-inflammatory effects. A proposed model has previously hypothesized that acupuncture might downregulate proinflammatory neuropeptides, proinflammatory cytokines, and neurotrophins, modulating transient receptor potential vallinoid (TRPV1), a G-protein coupled receptor which plays a central role in allergic rhinitis. Recent research has been largely supportive of this model. New advances in research include the discovery of a novel cholinergic anti-inflammatory pathway activated by acupuncture. A chemokine-mediated proliferation of opioid-containing macrophages in inflamed tissues, in response to acupuncture, has also been demonstrated for the first time. Further research on the complex cross talk between receptors during inflammation is also helping to elucidate the mediators and signaling pathways activated by acupuncture.
CONTEMPORARY RESEARCH PERTAINING TO ACUPUNCTURE AND MIND-BODY THERAPIES
Compiled by Brendan Zachar, A.P.
Acupuncture’s efficacy in treating chronic pain conditions:
- A systematic review of 29 randomized trials (17,922 patients) found acupuncture effective for chronic pain and therefore a reasonable referral option. 1
- In the case of osteoarthritis the use of acupuncture is associated with significant reductions in pain intensity, improvement in functional mobility and quality of life…Current evidence supports the use of acupuncture as an alternative for traditional analgesics in patients with osteoarthritis. 2
Acupuncture’s efficacy the treatment of depression:
- Standard acupuncture as well as auricular acupuncture has often been prescribed for mental and emotional disorders, such as depression. In this particular study researchers demonstrated that 3 particular auricular acupuncture points stimulated with an active electrical current, over the course of 3 days, can improve various aspects of quality of life significantly and also increased HRV, a potential indicator for state of health. 3
Acupuncture’s efficacy in treating gastrointestinal disturbances:
- A review of studies from both Chinese and Western Medicine literature suggests acupuncture at ST-36 suppresses hyperfunction (as in diarrhea), and stimulates hypofunction (as in constipation) of the gut motility. 4
Acupuncture’s efficacy in treating gynecological disorders:
- In regards to dysmenorrhea woman who were experiencing painful menstruation were instructed to follow a once a week acupuncture treatment for one year. In this controlled trial, 10 of the 11 woman (90.9%) showed improvement and there was a reduction of 41% analgesic medication used. 5
Acupuncture’s efficacy in treating hypertension and lowering blood pressure:
- Acupuncture stimulation at meridian points pericardium 5-6 and Large Intestines 10-11 are effective at reducing reflex-induced hypertension, a visceral reflex of the sympathetic nervous system. Researchers in this study found that acupuncture elicits specific modulation effects in the endocrine system as well as in inhibiting the rostral ventrolateral medulla(rVLM). Overall researchers have uncovered several mechanisms that might be involved in the long-lasting inhibitory action of acupuncture in hypertension. 6
- In a study of 65 patients with both stage I and II hypertension acupuncture resulted in a hypoaldosteronemic effect, which showed statistical correlation with a decrease in blood pressure. These results suggest that acupuncture has a therapeutic role in the treatment of hypertension. 7
- Acupuncture administered in the auricle as well as standard points administered on 360 patients produced a hypotensive effect on patients with essential hypertension. The effect was noted on 82% of patients to reduce excretion of adrenaline, inhibit plasma renin, and normalize lipid metabolism. The hypotensive effect in the majority of patients persisted for 12 months. 8
Acupuncture’s efficacy in treating migraine headaches:
- The results of this study showed a clinically relevant decrease in MMP-2 activity in patients with migraine treated with acupuncture. The mechanism underlying the effect of acupuncture in alleviating pain may be associated with a decrease in MMP-2 activity. 9
- A study found that acupuncture was equipotent to that of the pharmaceutical metoprolol in the reduction of frequency and duration of migraine attacks, and had fewer negative side-effects. 10
Acupuncture’s efficacy in treating multiple sclerosis:
- A demyelinating disease such as multiple sclerosis is a condition where the protective and conductive sheath that wraps around a nerve bundle is damaged. In a experimental Japanese study on rats researchers investigated whether EA(Electro Acupuncture) performed on the governing meridian could efficiently promote increase in cell number of OPCs or Oligodendrocyte precursor cells. OPCs are one of the potential treatment tools for dealing with multiple sclerosis. After 15 days of treatment with EA, NT-3 a neutrotrophic factor in NGF(Nerve Growth Factor) as well as NG-2 positive OPCs were significantly increased suggesting that EA treatment can promote remyelenation in a demyelinated spinal cord. 11
Acupuncture’s efficacy in treating post-stroke disorders:
- Meta-analysis results showed that twelve studies reported significant effects of Baihui (GV20)-based scalp acupuncture for improving infarct volume compared with middle cerebral artery occlusion group (P < 0.01), and thirty-two studies reported significant effects of Baihui (GV20)-based scalp acupuncture for improving the neurological function score when compared with the control group (P < 0.01). In conclusion, Baihui (GV20)-based scalp acupuncture could improve infarct volume and neurological function score and exert potential neuroprotective role in experimental ischemic stroke. 12
- A meta analysis of 24 systemic reviews concluded that acupuncture may be effective for post-stroke dysphagia, or trouble swallowing. Performance on the video-fluoroscopic swallowing study test often reported that acupuncture was superior to the control treatment. 13
Acupuncture’s efficacy in treating sleep disorders:
- The aim of this study was to examine the subjective self-reported sleep quality of post-menopausal women and cardiac sympathovagal activity after receiving auricular acupressure therapy. A group of 45 women having had insomnia for several years were treated with a course of 5 auricular points every night before going to sleep for 4 weeks. The study concluded that after 4 weeks, total sleep duration and efficiency were increased as well as the length of time it takes to accomplish the transition from full wakefulness to sleep. The research team suggested that the auricular acupressure intervention lead to more cardiac parasympathetic and less cardiac sympathetic activity, which contributed to an overall improvement in post-menopausal insomnia. 14
Acupuncture’s efficacy in treating tinnitus:
- This controlled study aimed to assess how acupuncture, stretching, and posture training could benefit somatically related tinnitus. The researchers found a significant reduction in the severity of tinnitus in the treatment group, both after treatment and on a follow-up after 3 months. The team gathered that this method may be a useful alternative to somatosensory tinnitus. 15
Acupuncure and adenosine release:
- Adenosine mediates the effects of acupuncture and that interfering with adenosine metabolism may prolong the clinical benefit of acupuncture. 16
Acupuncture and the biochemical importance of needle manipulation:
- The interstitial adenosine concentration increased significantly during acupuncture and remained elevated for 30 minutes after the acupuncture. Acupuncture-mediated adenosine release was not observed if acupuncture was not delivered in the Zusanli point or if the acupuncture needle was inserted, but not rotated. 17
Acupuncture and neuronal specificity:
- This study investigated the specific brain regions that were activated with fMRI (functional magnetic resonance imaging) while the researchers stimulated specific [EA] electroacupuncture points. The study illustrated that different areas of the brain were activated based on point specificity as well as needle depth and sensitivity applied. Specifically, they concluded that EA at analgesic acupoints of same meridian maybe involved the pain-related neuromatrix especially the hypothalamus-limbic system; deep EA at meridian points could elicit stronger needling sensation and modulate the pain-related neuromatrix more effectively than EA at nonmeridian points or shallow EA at meridian points. 18
- Few have investigated how acupuncture stimulated brain regions interacted at the whole brain level. A team of researchers with the help of brain scan technology divided the whole brain into 90 regions and analyzed functional connectivity following acupuncture at specific points. Their findings demonstrated that acupuncture at different acupoints may exert different modulatory effects on the post-stimulus resting brain, providing new evidences for the relatively function-oriented specificity of acupuncture effects. 19
- Many studies have attempted to demonstrate specific acupuncture effects vs non-specific acupuncture effects, such as those that generate effects based solely on expectation, context, and conditioning. This study illustrates that real acupuncture has a specific physiological effect and additionally that patients’ expectation and belief regarding a potentially beneficial treatment modulate activity in component areas of the reward system. 20
Acupuncture meridian-network research:
One of the most important concepts in Chinese Medical Theory is that of the meridians or organ-channel system. These channels are believed to be functional networks that course over the body into specific regions, organs, and bodily systems. Meridians are said to represent or reflect the health of various organ systems and it is understood that when these networks become compromised, disease may arise. Although the meridian system has never been proven by modern scientific methods there have been several interesting studies determined to find evidence for there existence.
- Researchers from the China Academy of Medical Sciences performed a controlled experiment on pigs by injecting a gel into acupuncture points that were situated along the stomach channel. The experiment was intended to block the flow of information or energy in this meridian, and over the course of several weeks, examine any changes in the animal and especially to the stomach organ. The researchers concluded that the pigs with the gel injected had numerous pathologies, such as bloated stomach/intestines when compared to the control group, which only had saline injected. The team believed that the results of this experiment demonstrates that obstruction along the stomach channel pathway can influence the state of the stomach and intestine, specifically to distention of these organs. 21
Acupuncture therapy and childbirth:
- The aim of this study was to determine the extent of acupuncture’s influence on the duration of labor. This controlled study determined that women who received acupuncture had 70% more Oxytocin during the first stage of labor, and 44% more during the second stage. Oxytocin is an important hormone that is released in large amounts during labor and helps facilitate child birth. Researchers concluded acupuncture is a recommended form of childbirth preparation due to its positive effect on the duration of labor, namely shortening the first stage. 22
- Acupuncture treatment during labor significantly reduced the need of epidural analgesia. Participants who received acupuncture assessed a significantly better degree of relaxation compared with the control group. The results suggest that acupuncture could be a good alternative or complement to those parturients who seek an alternative to pharmacological analgesia in childbirth. Further trials with a larger number of patients are required to clarify if the main effect of acupuncture during labour is analgesic or relaxing. 23
Acupuncture therapy and heart rate variability(HRV):
- Heart rate variability (HRV) is a way to measure beat-to-beat fluctuations in the heart rhythm. A low HRV score has been associated with an increased risk to mortality and a broad range disease marker, whereas a high HRV score seems to suggest increased synchronization between the two branches of the autonomic nervous system and entrainment between multiple body systems. There is strong evidence from randomized placebo controlled studies that acupuncture therapy modulates HRV, which can be used to monitor future treatment efficacy and research methods. 24
- Researchers conducted a study based upon the concept that vagal withdrawal and an overactive sympathetic nervous system can be potentially dangerous to the human body. They chose Sishencong points located around the apex of the skull to conduct a controlled study vs sham points around the periphery. Researchers concluded that manual acupuncture at the Sishencong points enhanced cardiac vagal activity and suppressed sympathetic activities in humans. They believe the underlying mechanisms and potential applications warrant further study. 25
- Real acupuncture at LI4 acupoint lead to a specific change in EEG frequency and in HRV parameters. This relationship was greater in real acupuncture 80% vs 45% and suggests a linear relationship between EEG frequency and HRV. 26
Auricular Acupuncture:
- A branch of the vagus nerve forms a bridge between a circumscribed area of the auricle, the external auditory meatus and an internal organs. These vagal reflexes have shown activity in autonomic functions of cardiovascular, respiratory, and gastrointestinal systems. Further studies have suggested projections from the auricular branch of the vagus nerve (ABVN) form the anatomical basis for vagal regulation in auricular acupuncture. 28
- Stimulation at auricular heart point regulates cardiovascular function by activation of baroreceptor sensitive neurons. 29
Chronic Stress:
- Chronic psychological stress appears to accelerate biological aging, and oxidative damage is an important potential mediator of this process. This study supports the emerging model that chronic stress exposure promotes oxidative damage through frequent and sustained activation of the hypothalamic-pituitary-adrenal axis. It also supports the less studied model of ‘eustress’ – that manageable levels of life stress may enhance psychobiological resilience to oxidative damage. 30
Compassion:
- The authors of this study investigated the effects of cross-group friendships and propose that friendly contact with members of different religious, cultural, ethnic, and racial groups reduce prejudices. The mechanism established for this seems to be self-disclosure, a type of transparent openness, via empathy, contact, and intergroup trust. 31
Heart Rate Variability:
Heart rate variability(HRV) measures autonomic modulation of the heart. A coherent HRV pattern is associated with an increased synchronization between the two branches of the ANS. It is postulated that a high HRV scores reflect a healthy coherence pattern within sympathetic and parasympathetic systems and may be a marker for healthy and resilient autonomic function.
- Decreased HRV has shown a predictive value of certain disease patterns among healthy adults. It has been a well-established risk factor for arrhythmic events and mortality among post-myocardial-infarction patients. Decreased HRV identifies diabetic patients with autonomic neuropathy. 32
Meditation:
Meditation is a popular arena of research as there have been many claims for health and mood improvements associated with its use. The scope of meditation practice is vast and encompasses many different forms, styles, and techniques; however, experienced meditators often have a particular intention, focus, or goal such as increasing attention, relaxation, or clarity during a given meditation. Still, many styles advice the practitioner to just be aware of their surroundings and not to have any specific goal or desire, perhaps just simply sitting or standing quietly aware of their surroundings. Research seems to suggest that even brief periods of meditation can improve memory, mood, and cognitive abilities.
- Researchers examined whether brief meditation training affected cognition and mood compared to a control group. Meditation improved mood and reduced fatigue and anxiety as well as significantly improved visuo-spatial processing, working memory, and executive functioning. Additionally 4 days of meditation training can enhance the ability to sustain attention. 33
- Researchers studied a basic form of concentration meditation in which sustained attention is focused on a small stimulus such as the breath while the brain was examined with the help of fMRI. Researchers found that a region of the brain that is typically involved in sustained attention was activated in advanced meditators more so than novice ones. Additionally, in response to distractor sounds advanced meditators had more activation in regions related to response inhibition and attention. 34
- Gamma waves are patterns of neural oscillations that occur in the brain and may be implicated in what we consciously perceive as “unity”. In this study, long-term Buddhist practitioners self-induce sustained high-amplitude gamma-band oscillations during meditation. Data suggests that mental training involves mechanisms that may induce short-term and long-term brain changes. 35
- Researchers concluded that through mental training, increased control over the distribution of limited brain resources may be possible. Additionally the team confirms that individuals practicing advanced meditation have a greater ability to detect subtle changes, not only in themselves, but also in the environment. 36
Negative Emotional State:
It has long been suggested in medical literature that negative emotions may contribute to a wide range of disease patterns. Research is emerging that illustrates just how emotional states such as: anger, fear, and pessimism can contribute in the course of a disease.
- This study discusses perspectives from psychoneuroimmunology on how negative emotions can intensify a variety of health threats. Negative emotions may have a course of onset starting from the immune system; inflammation has been linked to conditions such as aging, osteoporosis, arthritis, type 2 diabetes, certain cancers, Alzheimer’s disease, fraility and functional decline, and periodontal disease. Production of proinflammatory cytokines that influence these conditions can be stimulated by stress events and negative emotions. 37
- There is a correlation between the expression of anger and hostility and lessened nocturnal blood pressure “dipping”, that is individuals will experience higher blood pressure over the course of a night. Additionally, these emotional traits increase the risk of developing cardiovascular and cerebrovascular disease. 38
- The very act of listening to an angry speech, specifically its rhythm and intonation can illicit parts of the brain to mirror the content of the speaker. 39
- Violent media consumption, the act of watching violence portrayed in the news make participants react slower to happiness and faster to depictions of anger. It is postulated that participants “consuming” this type of media will feel more aggressive, angry, negative, and powerless. 40
- Negative emotions such as negative remarks and memories seem to have a stronger influence when compared to positive emotions in a wide range of cognitive domains. On the bright side of this study however are instances where positive emotions and motivational shifts are happening in older adults. 41
Oxytocin:
- Oxytocin is a hormone secreted by the pituitary gland and modulates several functions within the human body including increasing positive behavior and social bonding. In a study that investigated relationships among married couples and wound healing researchers concluded that higher levels of oxytocin in the blood were associated with more positive communication and faster wound healing. 42
Pharmaceuticals in the treatment of depression:
- In the last several years studies have been conducted to determine the efficacy of pharmaceutical preparations in the treatment of depression. 2,318 patients were grouped into a double-blind study and were randomly assigned either an anti-depressant or a placebo pill. The results of the study indicated a high correlation between the placebo effect and the drug effect, indicating perhaps that variation in drug effect was due to placebo characteristics of the studies. Researchers concluded that approximately one-quarter of the specific responses are from active-ingredients, half from placebo, and once-quarter from other “non-specific” factors. 43
Somatovisceral reflexes:
Somatovisceral reflexes are nerve reflexes that carry a signal from a stimulated sensory organ, towards the central nervous system, and finally towards the stimulated effector organ. According to studies these phenomena have been demonstrated in sites such as the gastrointestinal tract, urinary bladder, adrenal medula, lymphatic tissues, heart and vessels of the brain and peripheral nerves. Although the author of this study clearly makes no claim to extrapolate clinical situations from these findings, it is interesting to imagine future research studies that may demonstrate reflex mechanisms in the fields of osteopathic, chiropractic, and acupuncture therapies and perhaps reveal some of the diverse systemic effects attributed to these reflexive methods. 44
Vagal tone:
Vagal tone is the state of activity or passivity of the vagal nerve, a key component of our autonomic nervous system. Having high vagal tone is considered beneficial as it represents the dynamic functioning of the parasympathetic nervous system. Diminished activity of the vagas and its corresponding PNS functions is considered low vagal tone.
- A team of researchers hypothesized that low vagal tone is associated with impaired post stress recovery of cardiovascular, endocrine, and immune markers. Vagal tone was initially measured by measuring heart rate variability in both test and control subjects and by later comparing the two groups after a stress test. The data suggests that low vagal tone was associated with impaired recovery of cardiovascular, endocrine, and immune markers in healthy males. Additionally they concluded resting HRV can be used as a marker for future cardiovascular and stress related disease. 45
Bibliography
- Vickers, A. J. et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch. Intern. Med. 172, 1444–1453 (2012).
- Manyanga, T. et al. Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. BMC Complement Altern Med 14, 312 (2014).
- Shi, X. et al. Continuous Auricular Electroacupuncture Can Significantly Improve Heart Rate Variability and Clinical Scores in Patients with Depression: First Results from a Transcontinental Study. Evid Based Complement Alternat Med 2013, (2013).
- Li, Y., Tougas, G., Chiverton, S. G. & Hunt, R. H. The effect of acupuncture on gastrointestinal function and disorders. Am. J. Gastroenterol. 87, 1372–1381 (1992).
- Helms, J. M. Acupuncture for the management of primary dysmenorrhea. Obstet Gynecol 69, 51–56 (1987).
- Zhou, W. & Longhurst, J. C. Neuroendocrine mechanisms of acupuncture in the treatment of hypertension. Evid Based Complement Alternat Med 2012, 878673 (2012).
- Anshelevich, I. V., Merson, M. A. & Afanas’eva, G. A. [Serum aldosterone level in patients with hypertension during treatment by acupuncture]. Ter. Arkh. 57, 42–45 (1985).
- Akhmedov, T. I., Vasil’ev, I. M. & Masliaeva, L. V. [The hemodynamic and neurohumoral correlates of the changes in the status of hypertension patients under the influence of acupuncture]. Ter. Arkh. 65, 22–24 (1993).
- Cayir, Y. et al. Acupuncture decreases matrix metalloproteinase-2 activity in patients with migraine. Acupunct Med acupmed–2014–010612 (2014). doi:10.1136/acupmed-2014-010612
- Hesse, J., Møgelvang, B. & Simonsen, H. Acupuncture versus metoprolol in migraine prophylaxis: a randomized trial of trigger point inactivation. J. Intern. Med. 235, 451–456 (1994).
- Huang, S.-F. et al. An experimental electro-acupuncture study in treatment of the rat demyelinated spinal cord injury induced by ethidium bromide. Neurosci. Res. 70, 294–304 (2011).
- Wang, W., Xie, C., Lu, L. & Zheng, G. A systematic review and meta-analysis of Baihui (GV20)-based scalp acupuncture in experimental ischemic stroke. Sci. Rep. 4, (2014).
- Zhang, J.-H., Wang, D. & Liu, M. Overview of systematic reviews and meta-analyses of acupuncture for stroke. Neuroepidemiology 42, 50–58 (2014).
- Kung, Y.-Y., Yang, C. C. H., Chiu, J.-H. & Kuo, T. B. J. The relationship of subjective sleep quality and cardiac autonomic nervous system in postmenopausal women with insomnia under auricular acupressure. Menopause 18, 638–645 (2011).
- Latifpour, D. H., Grenner, J. & Sjödahl, C. The effect of a new treatment based on somatosensory stimulation in a group of patients with somatically related tinnitus. Int Tinnitus J 15, 94–99 (2009).
- Goldman, N. et al. Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nat Neurosci 13, 883–888 (2010).
- Takano, T. et al. Traditional acupuncture triggers a local increase in adenosine in human subjects. J Pain 13, 1215–1223 (2012).
- Zhang, J.-H. et al. Neuronal specificity of needling acupoints at same meridian: a control functional magnetic resonance imaging study with electroacupuncture. Acupunct Electrother Res 32, 179–193 (2007).
- Feng, Y. et al. Investigation of acupoint specificity by whole brain functional connectivity analysis from fMRI data. Conf Proc IEEE Eng Med Biol Soc 2011, 2784–2787 (2011).
- Pariente, J., White, P., Frackowiak, R. S. J. & Lewith, G. Expectancy and belief modulate the neuronal substrates of pain treated by acupuncture. Neuroimage 25, 1161–1167 (2005).
- Zhou, W.-T. et al. Pathological Changes in Internal Organs after Blocking Low Hydraulic Resistance Channels along the Stomach Meridian in Pigs. Evidence-Based Complementary and Alternative Medicine 2013, e935687 (2013).
- Zeisler, H., Tempfer, C., Mayerhofer, K., Barrada, M. & Husslein, P. Influence of acupuncture on duration of labor. Gynecol. Obstet. Invest. 46, 22–25 (1998).
- Ramnerö, A., Hanson, U. & Kihlgren, M. Acupuncture treatment during labour–a randomised controlled trial. BJOG 109, 637–644 (2002).
- Anderson, B., Nielsen, A., McKee, D., Jeffres, A. & Kligler, B. Acupuncture and heart rate variability: a systems level approach to understanding mechanism. Explore (NY) 8, 99–106 (2012).
- Wang, J. D., Kuo, T. B. J. & Yang, C. C. H. An alternative method to enhance vagal activities and suppress sympathetic activities in humans. Autonomic Neuroscience: Basic and Clinical 100, 90–95 (2002).
- Streitberger, K. et al. Effects of Verum Acupuncture Compared to Placebo Acupuncture on Quantitative EEG and Heart Rate Variability in Healthy Volunteers. The Journal of Alternative and Complementary Medicine 14, 505–513 (2008).
- Engel, D. The gastroauricular phenomenon and related vagus reflexes. Arch Psychiatr Nervenkr 227, 271–277 (1979).
- He, W. et al. Auricular Acupuncture and Vagal Regulation. Evid Based Complement Alternat Med 2012, (2012).
- Gao, X. Y. et al. Acupuncture-like stimulation at auricular point Heart evokes cardiovascular inhibition via activating the cardiac-related neurons in the nucleus tractus solitarius. Brain Res. 1397, 19–27 (2011).
- Aschbacher, K. et al. Good stress, bad stress and oxidative stress: Insights from anticipatory cortisol reactivity. Psychoneuroendocrinology 38, 1698–1708 (2013).
- Turner, R. N., Hewstone, M. & Voci, A. Reducing explicit and implicit outgroup prejudice via direct and extended contact: The mediating role of self-disclosure and intergroup anxiety. J Pers Soc Psychol 93, 369–388 (2007).
- Stein, P. K. & Kleiger, R. E. Insights from the study of heart rate variability. Annu. Rev. Med. 50, 249–261 (1999).
- Zeidan, F., Johnson, S. K., Diamond, B. J., David, Z. & Goolkasian, P. Mindfulness meditation improves cognition: evidence of brief mental training. Conscious Cogn 19, 597–605 (2010).
- Brefczynski-Lewis, J. A., Lutz, A., Schaefer, H. S., Levinson, D. B. & Davidson, R. J. Neural correlates of attentional expertise in long-term meditation practitioners. PNAS 104, 11483–11488 (2007).
- Lutz, A., Greischar, L. L., Rawlings, N. B., Ricard, M. & Davidson, R. J. Long-term meditators self-induce high-amplitude gamma synchrony during mental practice. Proc. Natl. Acad. Sci. U.S.A. 101, 16369–16373 (2004).
- Slagter, H. A. et al. Mental Training Affects Distribution of Limited Brain Resources. PLoS Biol 5, e138 (2007).
- Kiecolt-Glaser, J. K., McGuire, L., Robles, T. F. & Glaser, R. Emotions, morbidity, and mortality: new perspectives from psychoneuroimmunology. Annu Rev Psychol 53, 83–107 (2002).
- Thomas, K. S., Nelesen, R. A. & Dimsdale, J. E. Relationships between hostility, anger expression, and blood pressure dipping in an ethnically diverse sample. Psychosom Med 66, 298–304 (2004).
- Sander, D. et al. Emotion and attention interactions in social cognition: brain regions involved in processing anger prosody. Neuroimage 28, 848–858 (2005).
- Kirsh, S. J., Mounts, J. R. W. & Olczak, P. V. Violent media consumption and the recognition of dynamic facial expressions. J Interpers Violence 21, 571–584 (2006).
- Kisley, M. A., Wood, S. & Burrows, C. L. Looking at the sunny side of life: age-related change in an event-related potential measure of the negativity bias. Psychol Sci 18, 838–843 (2007).
- Gouin, J.-P. et al. Marital behavior, oxytocin, vasopressin, and wound healing. Psychoneuroendocrinology 35, 1082–1090 (2010).
- Kirsch, I. & Sapirstein, G. Listening to Prozac but hearing placebo: A meta-analysis of antidepressant medication. Prevention & Treatment 1, No Pagination Specified (1998).
- Sato, A. Somatovisceral reflexes. J Manipulative Physiol Ther 18, 597–602 (1995).
- Weber, C. S. et al. Low vagal tone is associated with impaired post stress recovery of cardiovascular, endocrine, and immune markers. Eur. J. Appl. Physiol. 109, 201–211 (2010).
How can Western medicine and Chinese medicine describe the body in such different ways and both be correct?
It is important to grasp that one cannot understand Traditional Chinese Medicine by trying to explain it in Western scientific or medical terms. The ancient Chinese physicians developed a system of medicine that has survived for over three thousand years. Chinese medicine is complete within itself but that it is based on physiological concepts, theories regarding cause of disease, methods of diagnosis, and principles of treatment that are completely different from the western way of viewing the body.
One way to understand how two medical systems can view the body differently without one system being “right” and the other system being “wrong” is to use the analogy of a map. For example, compare a road map and a topographical map of the city of Waco. Both maps represent the same area, but they do so in very different ways. As long as both maps are based on accurate information, serve as useful tools for their intended purposes, and have been created with self-consistent logic, it would be absurd to claim that one map is more “correct” than the other. The maps are different because they are intended to serve different purposes. If you were planning a road trip from Waco to Denver, you would use the road map. On the other hand, if you were attempting to determine which area of the city was subject to flooding, a topographical map would be a more useful tool.
Both Western and Chinese medicine provide a “map” for understanding the human body in health and disease. Western medicine is like the road map. Depending on the size and scale of the map, a road map can offer very detailed representation of countries, states, counties, cities, neighborhoods, and even individual buildings. If you were using a map to select the shortest route to an appointment across town, you would choose one with quite a small scale and then you would disregard parts of the map that did not pertain the roads and highways that you plan to use. This is similar to the way that Western medicine views the body – as a collection of distinct parts (organs, tissues, cells) that can be taken apart and considered in isolation. Diagnosis and treatment of disease in Western medicine involves using signs, symptoms, and various diagnostic tests to pinpoint the disordered part(s) of the body and then counteract these signs and symptoms with medications, surgery, or other techniques.
In contrast, Chinese medicine is like a topographical map. On this type of map, mountains, valleys, hills, and plains are defined only in relationship to one another. It is impossible to separate the various pieces of the landscape and still maintain a meaningful representation of the whole. From the viewpoint of Chinese medicine, no single sign, symptom, or body part can be understood except within the context of the whole patient. In establishing a diagnosis and treatment plan, the Chinese medicine practitioner searches for and organizes many signs and symptoms (including many that a Western physician would consider irrelevant or unimportant) and subsequently identifies a “pattern of disharmony”. In Chinese thought, there is no single cause of disease, rather it is the interaction of numerous factors in the patient’s life (climate, diet, physical activity, contagious diseases, excessive emotions, inherited constitution, trauma, and others) that results in imbalance (also called disharmony). Eventually this imbalance results in the signs and symptoms of disease.
Are you suggesting that Chinese medicine is better than Western medicine or that I should stop seeing my M.D.?
Absolutely not. Modern Western medicine has changed the world by achieving many amazing triumphs over disease, and Western medicine is the best choice when it comes to the treatment of acute infections, traumatic injury, situations which require surgery, and other illnesses such as cancer. Fortunately, Western medicine has tools at its disposal to actually cure these conditions by killing bacteria, repairing traumatic injury, repairing congenital or acquired malformation of organs or tissues, and stopping the spread of malignant tumors.
On the other hand, most physicians will admit that there are a number of health problems that are not addressed particularly well by modern Western medicine. In the case of many chronic diseases and disorders, Western medicine offers only palliative care – meaning that symptoms are temporarily relieved with medication or surgery but the underlying cause remains. Examples of such chronic conditions include allergies, asthma, insomnia, depression, anxiety, chronic fatigue, PMS, menstrual pain and irregularity, back pain, attention deficit disorder (ADD), and many others. In these cases, Chinese medicine offers a mode of treatment that effectively addresses the root cause of the disorder, while at the same time alleviating symptoms. In many cases, Chinese medicine can be used very effectively as an adjunct or complement to conventional Western care.
My background in both Chinese medicine and Western science uniquely qualifies me to offer patients the best of both worlds.
The following video shows how Western and Chinese medicine can be used together for the patient’s benefit.
What are Qi, Yin, and Yang?
Qi
“And the LORD God formed man of the dust of the ground, and breathed into his nostrils the breath of life and man became a living soul.”
– Genesis 2:17
“The spirit of God made me, and the breath of the Almighty gave me life.”
– Job 33:4
“Qi is understood to be the intrinsic, dynamic, self-regulating and self-maintaining power of the organism. All healing in Chinese Medicine is directed, ultimately, at conserving, protecting, augmenting, restoring, and facilitating Qi.”
– Between Heaven and Earth by Harriet Beinfield and Efrem Korngold
“Concerning matter; we have been all wrong. What we have called matter is energy whose vibration has been so lowered as to be perceptible to the senses. There is no matter.”
– Albert Einstein
“If you want to find the secrets of the universe, think in terms of energy, frequency, and vibration.”
– Nikola Tesla
A cross-cultural concept
Numerous cultures throughout history have identified a certain “vital energy” as critical for life and health. The Chinese referred to this energy as Qi, the Japanese called it Ki, and in Hebrew the term was “Ruach” (which can be translated as breath, wind, or spirit – see Genesis 2:17 above). It is this breath of life that God breathed into dust to create man. In the Bible, God is the source of Ruach (see Job 33:4, above). In human beings, Ruach further denotes an animating dynamic that is characterized by reason, will, and conscience. More recently, European physicians and scientists have called this vital energy Elan Vital or Orgone Energy.
What does Qi do?
Qi is the motive force behind your ability to move, see, hear, heal, digest, speak, love, and dream. It is the “spark” that keeps your heart beating, your blood circulating, and your brain thinking. It is the energy behind the phenomenal growth of a small child and the remarkable ability of the human body to heal from injury and disease. One translation of the word Qi is “that which animates life”—the presence of Qi is what distinguishes a living being from an inanimate object. The balanced, unobstructed flow of Qi is critical for health. Qi serves 5 major functions:
- Activates and animates (metabolic function)
- Warms the body (thermogenic function)
- Protects and defends (immune function)
- Transforms and transports (digestive function)
- Contains and retains (circulatory function)
Meridians (also known as channels) are the pathways that conduct Qi throughout the body
Free flow along the fourteen major and innumerable minor meridians of the human body brings life-giving Qi to every cell of the body, including the muscles, nerves, and organs. An obstruction in a meridian is like a dam in a river or a kink in a hose – Qi builds up and overflows the normal boundaries of the meridian on one side; on the other side tissues lack nourishment. When there is an obstruction, energy stagnates on either side of the blockage and tissue function is impaired. If the blockage is sustained, pain and disease results. In Chinese there is a saying,
“If there is pain, there is no free flow; if there is free flow, there is no pain.”
Blockages can be caused by injury, contagious diseases, emotional stress, lack of physical activity, excessive physical activity, overuse injuries, faulty diet, and many other factors. Acupuncture and Chinese herbal medicine are used to remove blockages, regulate Qi, and restore physiological and psychological equilibrium.
Yin and Yang
Yin and Yang is a concept based on the simple observation of the ancient Chinese people that everything in nature exists somewhere on a continuum between two opposite poles and many things in nature dynamically alternate between these two poles. For example, day (yang) turns into night (yin), summer (yang) turns into winter (yin), growth (yang) turns into decay (yin). Yin and yang are opposite yet interdependent forces – one cannot exist without the other. For example, there can be no cold without heat, no dryness without moisture, no activity without rest. In the human body there is both yin Qi and yang Qi, just as in nature water can exist both in the form of ice (yin) or steam (yang). In the human body, health is defined as a dynamic balance between yin and yang. Disease results when the body is unable to maintain equilibrium in response to internal and external fluctuations in the environment. Stimulation of acupuncture points restores the appropriate yin/yang balance in the meridians and enhances the ability of the body to maintain this equilibrium. By the age of 40, half of the body’s yin has been consumed. (This is because our modern lives tend to burn yin energy much more quickly than yang energy. We are always busy, rarely rest, rely heavily on technology, and our minds are almost never quiet. All of these things consume yin.) This lack of cooling, moisturizing energy results in a relative excess of warming, drying yang energy. This imbalance is frequently referred to as “deficiency heat”. This is a commonly encountered phenomena in women as they age and approach menopause. As the yin becomes more and more deficient, women often develop symptoms such as night sweats, hot flashes, vaginal dryness, insomnia, and anxiety. These are all signs of yin deficiency – indications that there is not adequate yin to cool and moisturize the body tissues. Fortunately, this situation can be remedied with simple dietary, lifestyle, and herbal strategies.
Blood
In Chinese medicine, the term “Blood” refers to the western idea of blood (red liquid that flows in the circulatory system), as well as several additional functions. From the Chinese point of view, Blood is actually a form of denser, more material Qi. Blood flows in the veins and arteries, but it also flows in the meridians (along with Qi). Blood and Qi cannot be separated; Qi infuses life into Blood and without Qi, Blood would be an inert fluid. In the most basic terms, Blood is the substance that serves to nourish and moisten every cell in the body. According to Chinese medical theory, Blood serves several major functions:
- Nourishes the body
- Moistens the tissues
- Forms the material foundation for the mind (when there is Blood deficiency, a person experiences “deficient restlessness”, which includes vague anxiety, slight irritability, and a feeling of dissatisfaction.)
Essence
Just as Blood is denser than Qi, Essence is denser than Blood. According to Bob Flaws, “Essence is the most fundamental, essential material the body uses for its growth, maturation, and reproduction.” There are two forms of Essence. The Pre-Heaven Essence is inherited from our parents and is formed at the time of conception. It is stored in the Kidney, which forms the foundation for the function of all the other internal organs. The concept of Pre-Heaven Essence corresponds roughly to the western notion of genetics and it determines our basic constitution, strength, and vitality. We are each born with a finite amount of Pre-Heaven Essence and when it is gone, we die. The Pre-Heaven Essence could be likened to a long-term savings account. It is important for us to live in a way that protects this limited resource. “Fast living”, including poor diet, stress, too little sleep, caffeine, too much sex, drugs, and alcohol are factors that accelerate our expenditure of Pre-Heaven Essence. Living in a way that minimizes the withdrawals from our Pre-Heaven Essence Account is important for long-term health. This is especially important for individuals who are born with a limited amount of Pre-Heaven Essence (i.e. a weak constitution). Interestingly enough, the Hebrew word for “inner parts” in Psalm 139:13 refers to the kidney. This implies that more than one ancient culture saw the kidney as fundamental to human life.
“You made all the delicate, inner parts of my body and knit me together in my mother’s womb. Thank you for making me so wonderfully complex! Your workmanship is marvelous, and how well I know it. You watched me as I was being formed in utter seclusion, as I was woven together in the dark of the womb. You saw me before I was born. Every day of my life was recorded in your book. Every moment was laid out before a single day had passed.”
“You made all the delicate, inner parts of my body and knit me together in my mother’s womb. Thank you for making me so wonderfully complex! Your workmanship is marvelous, and how well I know it. You watched me as I was being formed in utter seclusion, as I was woven together in the dark of the womb. You saw me before I was born. Every day of my life was recorded in your book. Every moment was laid out before a single day had passed.”
The Post-Heaven Essence is formed on a daily basis from the food we eat, the liquids we drink, and the air we breathe. If the Pre-Heaven Essence is a long-term savings account, the Post-Heaven Essence is the checking account that we use for our day-to-day expenses. Fortunately, a strong Post-Heaven Essence that is formed from excellent diet, restful sleep, and proper exercise can partially make up for a weak constitution or past indiscretions. Because Essence forms the basis for reproduction, adequate reserves of Essence are critical for conception and healthy pregnancy. According to Chinese medicine, a baby conceived at a time when either parent is weakened by illness, fatigue, or old age is likely to be born with weak Pre-Heaven Essence, which will result in a weak constitution and a greater likelihood of congenital malformations or other health difficulties.
I don’t live near Waco. How can I find a qualified acupuncturist in my area?
As I have written about here, here, and here, the increased popularity, scientific acceptance, and positive media coverage of acupuncture has led to a growing number of unqualified practitioners jumping on the bandwagon to offer this therapy. As a prospective acupuncture patient, it is critically important for you to seek out a true expert, namely a licensed acupuncturist.
Unlike physical therapists, chiropractors, and physicians offering acupuncture/dry needling (having typically received between 30-100 hours of training, only a portion of which is hands-on practice), licensed acupuncturists have received a minimum of 660 hours of clinical training (many programs require much more than this — my degree program required 1080 hours of supervised clinical practice). This is in addition to between 1200-1800 hours of classroom instruction (my program required 1920 hours).
Fortunately it is not difficult to find a qualified acupuncturist in most cities. Here is a resource that you can use to locate an appropriately credentialed professional in your area: The National Certification Commission on Acupuncture and Oriental Medicine
